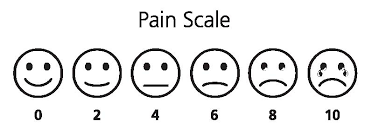
Pain is one of the most difficult things to quantify. The doctor can ask you: How would you classify the pain from 0 to 10, being 10 the most painful and 0 not painful? and you might answer with a number, but the scale is subjective. So far, there was no method to actually quantify pain. fMRI (functional MRI) might change that.
A recent study found a way to predict the pain intensity with fMRI. Basically, several volunteers (I'm not sure how much did this study paid, but I don't see myself volunteering for a pain study...) were scanned while thermal-induced pain was being applied. Using machine-learning techniques, the scientist found patterns of activity in the brain which increased when pain was applied. In this study, people who are going through break-ups were also invited to participated with the aim of finding common activated regions in physical and "social" pain. Finally, the effect of drugs for pain relieve was also studied.
OK, so now you can quantify my pain, then what? Well, just imagine that your pain prescription is not working so well, because your pain was under or over-estimated... or maybe the source of your pain is not being correctly identified...
There are infinite studies interesting to do, specially ones without any medical interest:
- What hurts more: giving birth or being kicked in the balls?
- Who is suffering more after the break-up: me or my partner? I already can imagine: "Look in this fMRI study how much you made me suffer!"
The full study can be read here:
Wager TD, Atlas LY, Lindquist MA, Roy M, Woo CW, & Kross E (2013). An fMRI-based neurologic signature of physical pain. The New England journal of medicine, 368 (15), 1388-97 PMID: 23574118
A recent study found a way to predict the pain intensity with fMRI. Basically, several volunteers (I'm not sure how much did this study paid, but I don't see myself volunteering for a pain study...) were scanned while thermal-induced pain was being applied. Using machine-learning techniques, the scientist found patterns of activity in the brain which increased when pain was applied. In this study, people who are going through break-ups were also invited to participated with the aim of finding common activated regions in physical and "social" pain. Finally, the effect of drugs for pain relieve was also studied.
OK, so now you can quantify my pain, then what? Well, just imagine that your pain prescription is not working so well, because your pain was under or over-estimated... or maybe the source of your pain is not being correctly identified...
There are infinite studies interesting to do, specially ones without any medical interest:
- What hurts more: giving birth or being kicked in the balls?
- Who is suffering more after the break-up: me or my partner? I already can imagine: "Look in this fMRI study how much you made me suffer!"
The full study can be read here:
Wager TD, Atlas LY, Lindquist MA, Roy M, Woo CW, & Kross E (2013). An fMRI-based neurologic signature of physical pain. The New England journal of medicine, 368 (15), 1388-97 PMID: 23574118
